The Premature Use Of Mechanical Ventilation In The First Wave Of The Covid Pandemic
The Premature Use Of Mechanical Ventilation In The First Wave Of The Covid Pandemic
The widespread and unprecedented initiation of mechanical ventilation early in the hospital course of Covid patients caused great harm. I am proud that I was able to block the practice at UW.
Pierre Kory, MD, MPAFeb 24
I would say that in all the Covid “rabbit holes” I have gone down, each one then led to me entering an often public “science battle,” only some of which I have “won.” But I did win a few, none more successful than when I immediately shut down the shocking and rapidly spreading obsessive practice by ER and ICU doctors with putting Covid patients on ventilators “early.”
As the Chief of the Critical Care Service and Medical Director of the Trauma and Life Support Center at the University of Wisconsin (we called the center “the TLC” for short but basically it was just the name for the main ICU at UW), I was one of the more experienced ICU clinicians. I was also known as a “vent geek.” In fact, one of the reasons why I became a pulmonary and critical care doc stemmed from an early fascination with operating mechanical ventilators. Subsequently, I have long taught taught the management of acute respiratory failure and mechanical ventilation to medical students, residents, and fellows. One of my core teaching points focused on identifying the optimal timing for the decision to transition a patient to a mechanical ventilator.
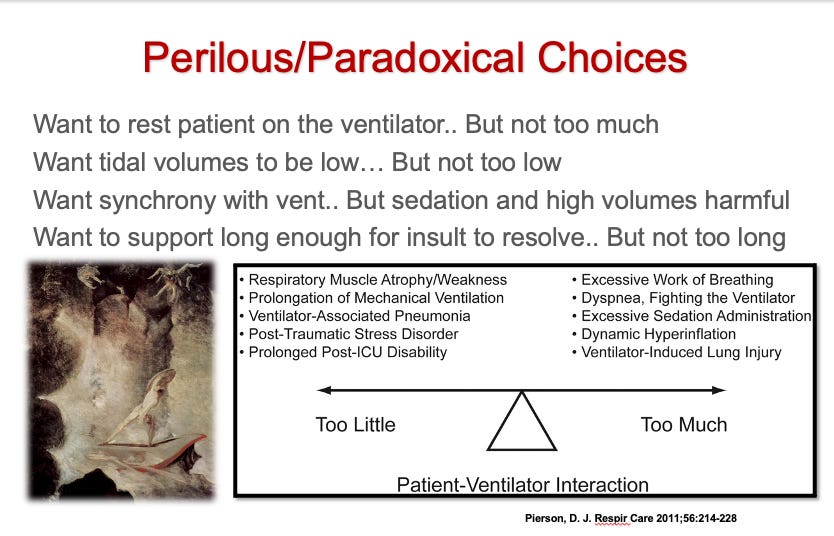
Guidance on how to make the decision is simple conceptually but stressfully complex in practice. Basically, the timing of transition to mechanical ventilation is that you always wants to shoot for “not doing it too early” while also “not delaying until too late.” See how simple that is?
The reason for this approach is that mechanical ventilators are “double edged swords” in that they can absolutely be life-saving when truly indicated (benefits outweigh risks), but they also can injure the lungs when used inexpertly or prematurely because by placing someone on a mechanical ventilator, this automatically worsens their prognosis as well as their time to recovery.
The worsened prognosis stems from the deleterious effects of mechanical ventilation which often requires prolonged sedation and immobility which then can cause confusion, delirium, muscle atrophy, and weakness. All of which prolongs patients recovery and opens them up to developing complications (the shorter time you spend in an ICU the better you will do).
So, the timing of the decision is critical – do it too early and you will be doing it unnecessarily in a proportion of cases, and doing it too late leads to a procedure with higher risks (the act of intubating someone in severe distress with low oxygen is much riskier than in a more stable patient). So knowing when to intervene when a patient’s respiratory status is deteriorating is a critical and challenging patient care issue.
This challenge is best described by Professor Martin J. Tobin whom I call the “Godfather” of mechanical ventilation given that he is the author of the “Bible” of mechanical ventilation, a 3-inch wide textbook called “Principles of Mechanical Ventilation.” It is the only medical textbook that I have read completely… twice. See, I told you I was a vent geek. Fun fact: Professor Tobin was the expert witness in the George Floyd criminal case while I was the expert witness in the civil case). Anyway, Dr. Tobin invokes the analogy of the mythical Greek sea monsters of Homer called Psylla and Charbybdis when he discusses how to “set” the mechanical ventilator properly, but I think the analogy applies just as well in regards to the timing and initiation of mechanical ventilation.
From Wikipedia:
Scylla and Charybdis were mythical sea monsters noted by Homer; Greek mythology sited them on opposite sides of the Strait of Messina between Sicily and Calabria, on the Italian mainland. Scylla was rationalized as a rock shoal (described as a six-headed sea monster) on the Calabrian side of the strait and Charybdis was a whirlpool off the coast of Sicily. They were regarded as maritime hazards located close enough to each other that they posed an inescapable threat to passing sailors; avoiding Charybdis meant passing too close to Scylla and vice versa. According to Homer's account, Odysseus was advised to pass by Scylla and lose only a few sailors, rather than risk the loss of his entire ship in the whirlpool.[3]
Because of such stories, the bad result of having to navigate between the two hazards eventually entered proverbial use.
Now, here are a couple of slides from one of my lectures on managing mechanical ventilators:
Similarly, knowing when to intubate someone (i.e. the act of sedating and paralyzing someone in order to insert a breathing tube through the vocal cords and into the trachea is a procedure that presents a rare but catastrophic risk).
Meaning that if you don’t establish a supportive airway quickly in some patients, a cardiac arrest can ensue. Fortunately, due to modern intubating techniques, equipment (video laryngoscopes), simulation training practices, and sedation and paralysis protocols, death is rare but still non-zero. Now, although death is quite rare, I have been involved in more stressful/scary intubation scenarios than I (or my patient) would have liked. “Managing a difficult airway” is the emergency of all emergencies because you have a patient still alive where you are responsible to prevent a cardiac arrest from deprivation of oxygen and/or excessive respiratory fatigue.
Certainly cardiac arrest resuscitations are emergencies, but the heart is already stopped and CPR is relatively straightforward in my opinion.. so it is a little different from the perspective of a physician. In one situation you are trying to bring someone back from an arrest while in the other you are trying to prevent its occurrence.
In every instance that I made a decision to put a patient on a ventilator, I would always reflect afterwards as to whether I felt I had done it too early or too late. Psylla or Charybdis. With rare exceptions, I generally felt like I did it too late (not late late, but generally beyond the time that it should have been clear that they were not going to be able to avoid the ventilator.)
The reason for my delaying is that I tried to give every patient as much time and treatment as I could until it was clear they were not improving enough or quickly enough to avoid it. But I tried to give them every possible chance without endangering them. So I would consider myself a “late intubator” by practice. The comfort level with deciding on the appropriate time to intubate obviously varies across physicians as their risk tolerance (and their perceptions of the competing risks) varies according to their training, experience, and personality.
I never forget one fellow I had when I was the Director of a Fellowship training Program back in New York who, during his three years of training had more than double the amount of intubations as any other fellow (although not the only reason, I did feel he was an “early intubator” and I tried to guide him to a more conservative approach before he graduated my program).
However, as Covid patients began to be admitted to UW Hospital, suddenly a number of my colleagues were coming up to me and “suggesting” that we institute a “rule” for when we put someone on a ventilator and they were suggesting that we use the amount of oxygen they were requiring. I immediately thought this was insane but I also understood where it was coming from – the doctors were scared as they had not developed familiarity with the disease and this was compounded by rumors or reports of Covid patients who were supposedly coming in with low oxygen levels and who, despite oxygen supplementation and looking fairly stable, would suddenly “crash.”
Although this suggestion well-intentioned as I believe the doctors were advocating for early intubation largely for the “safety” of the patient, I knew this would paradoxically spell disaster if the practice became standard. Plus, I had serious doubts a pneumonia/pneumonitis would cause “sudden crashes.”
Now, one of the main purposes of ICU’s are for “close monitoring” of patients who have single or multiple organ failures. I have spent my career consulting on patients in various forms and degrees of respiratory distress, and all respiratory failure conditions have a general trajectory and/or response to certain medicines such that knowing when to intubate becomes easier to identify as you gain more experience.
And I gained a ton of experience in my early career because when I got hired in my first job after fellowship training, my hospital was poorly staffed with pulmonologists and intensivists. In the first three years of my career I saw so many patients that my “billings” were causing concern by hospital leadership because I was seeing over 200% the amount of patients that an average full time intensivist would see in a year (which might suggest Medicare or Medicaid insurance fraud and thus trigger an audit – whatever). I worked 80-90 hours a week, plus I moonlighted overnight frequently so I gained a ton of experience (and expertise) fairly quickly.
Anyway, I simply refused to believe that an inflamed lung would lead to precipitous crashes and I knew this both intuitively but I also knew it from talking to my colleagues on the front lines in New York City. So I argued with the “early intubation” crowd that, even though this was a novel disease it doesn’t change the foundational principal of when to institute mechanical ventilation.
At the daily Covid briefing that I led each day at UW (attended in person and remotely by all residents, hospitalists, and intensivists in charge of taking care of COVID patients), I argued very strongly that we should avoid setting an arbitrary oxygen requirement limit for intubation. Some had suggested to intubate once a patient required more than 6 liters per minute of oxygen via nasal cannula while others were suggesting something higher. I explained that the indication for the institution of mechanical ventilation should never be based on an oxygen level and instead must be almost solely based on an assessment of the patients “work of breathing” and their ability to sustain that work of breathing. This is where it gets a bit more complicated as a patient’s ability to sustain an elevated work of breathing is itself dependent on multiple factors such as their frailty (or conversely their strength), their mental status, and the cause of their respiratory failure (some conditions are more easily and quickly reversed than others). Here is a schematic that I would use to try to teach this concept to my students (made by my old colleague Nate Sandbo at UW.)
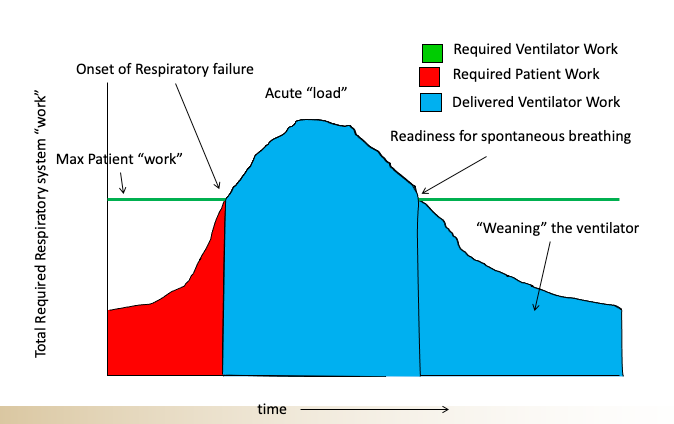
So when you look at a patient who is struggling to breathe you have to ask yourself, can they sustain that amount of effort, for how long, and what is the underlying cause and is it rapidly reversible? There are certain conditions like acute pulmonary edema which can sometimes be turned around quite quickly with diuretics and blood pressure management and something called a non-invasive ventilator (called BPAP or CPAP machines) such that even when patients are in significant distress, you sometimes have enough time to “turn them around” before they “crash.” Other conditions like a worsening pneumonia with sepsis, there the patients generally need to be intubated once significant signs of respiratory distress are observed given that in such patients the “turnaround” is not so quick and there is a higher mortality associated.
Anyway, my colleagues and trainees carefully listened and for maybe the first and last time in the pandemic, simply trusted my judgement and advice without too much “argument”. Whew. The idea of setting arbitrary oxygen limits as the trigger for intubation simply disappeared. I’m pretty damn proud of that because I know that was not the case around the country given that in many hospitals and academic medical centers they were using arbitrary limits to put patients on ventilators, and I believe this was one important factor which led to the widespread need for additional ICU rooms as well as ventilator shortages.
I must say however, that I do not believe this “early intubation” practice lasted very long as doctors quickly gained more experience in managing Covid patients. They began to recognize that the pulmonary phase of Covid presented as a relatively unique form of respiratory failure in that patients would come in with often quite low blood oxygen levels yet would appear fairly comfortable in terms of their work of breathing, a condition doctors started calling “happy hypoxia.”
Doctors then quickly got used to using high flow oxygen devices instead of mechanical ventilation. These devices, called “heated high flow nasal cannulas” (HHFNC) are a marvel of technology as you can deliver incredibly high flows of oxygen (up to 60 liters per minute) into their nose given that the oxygen is 100% humidified and heated. With normal low flow nasal cannulas that are not fully humidified or heated, if you try to increase the flow past 5 liters per minute, the patients cannot tolerate it due to discomfort and dryness. HHFNC became the workhorse of Covid and I believe many lives were saved by those devices. Fun fact: the devices were originally developed for use in racehorses (horses again?) and have only been applied to the care of patients in 1999, not falling into widespread use until after 2010.
Next post I will go a little deeper into the reasons why Covid patients presented with this phenomenon of “Happy Hypoxia” (for all you respiratory failure geeks).
P.S I just want to say thanks to all my subscribers, especially the paid ones! Your support is greatly appreciated as it allows me to devote what is often large amounts of time I spend researching and writing my posts, so again, thanks.
P.P.S. I opened a tele-health clinic with a specialized focus on the treatment of both Post-Vaccination injury and Long-Haul Covid syndromes. If anyone needs our help, feel free to visit our website at www.drpierrekory.com.
P.P.P.S. I am writing a book about what I have personally witnessed and learned during Pharma’s historic Disinformation war on ivermectin. Pre-order here for:



No comments:
Post a Comment